The trial was conducted by a cooperation between the University of Bristol and the National Health Service Blood and Transplant (NHSBT), a government body which oversees blood and organ transplants in the United Kingdom. They published their findings in the journal Nature Communications
Previously, scientists wishing to grow red blood cells relied on stem cells — but they were never able to produce very much.
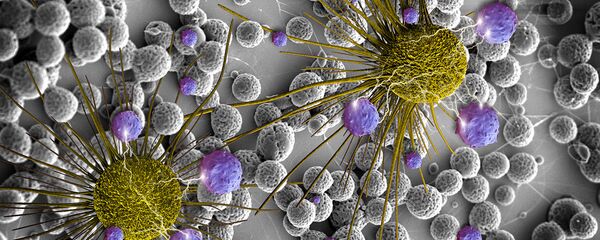
An erythroblast is an immature red blood cell; unlike mature cells, they have nucleuses. An erythroblast produces about 50,000 red blood cells, then dies — which is a problem, because a pint of blood contains 1 trillion red cells. The Bristol team successfully "immortalized" the erythroblasts, meaning they will continue to produce mature red blood cells indefinitely.
"Previous approaches to producing red blood cells have relied on various sources of stem cells which can only presently produce very limited quantities," Dr Jan Frayne with Bristol's School of Biochemistry said in a statement.
"By taking an alternative approach we have generated the first human immortalised adult erythroid line (Bristol Erythroid Line Adult or BEL-A), and in doing so, have demonstrated a feasible way to sustainably manufacture red cells for clinical use from in vitro culture… we've grown liters of it."
Growing red blood cells has numerous benefits. A cheap, reliable method of producing blood would not only help address the never-ending demand for donations, but would also reduce (or even eliminate) the risk of disease transmission during blood transfusions. After all, lab-grown blood is very unlikely to be carrying a bloodborne illness compared to donor blood. It would also allow for those with rare blood types to have easier access to transfusions.
"Scientists have been working for years on how to manufacture red blood cells to offer an alternative to donated blood to treat patients," said Professor Dave Anstee, Director of the research unit.
"The patients who stand to potentially benefit most are those with complex and life-limiting conditions like sickle cell disease and thalassemia, which can require multiple transfusions of well-matched blood. The intention is not to replace blood donation but provide specialist treatment for specific patient groups."
NHS Blood and Transplant has announced plans for human trials of their manufactured blood before the end of 2017. However, they will not be using the BEL-A blood, but instead manufactured red cells from stem cells collected from blood donations.
The team cautioned that large-scale production of artificial blood is still a far-away goal, with the purpose of BEL-A to be assist in donations. "There is a bioengineering challenge," said Anstee to the BBC. "To produce that much at scale is quite a challenge, and really the next phase of our work is to look at methods of expanding the yield."
The World Health Organization reports that roughly 108 million pints of blood are collected globally every year, but the majority of countries in the world have a higher demand for blood than supply.