A report published in March by the Armed Forces Health Surveillance Branch found that the incidence rate of chlamydia among servicemen and women doubled between 2013 and 2018. Gonorrhea rates among men doubled during the same time period, while among women, the disease spiked by 33%. Syphilis diagnoses among servicemen and women have also tripled compared to 10 years ago. However, not all STIs are increasing in prevalence among military members. The rates of incidence for genital herpes decreased slightly between 2010 and 2018, and cases of human papillomavirus (HPV) decreased by almost 52% during the same time period, most likely due to the widespread use of the HPV vaccine.
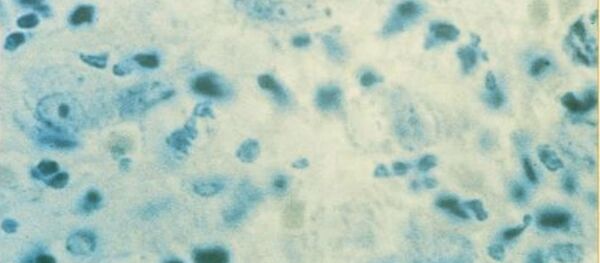
Chlamydia and gonorrhea are bacterial infections that often cause no symptoms. If left untreated, they can result in reproductive health problems, including pelvic inflammatory disease and infertility in women. Syphilis, also a bacterial infection, can also hijack the nervous system and lead to several serious symptoms, including difficulty coordinating muscle movements, paralysis, dementia and sensory deficits, according to the CDC. Syphilis can lead to very serious long term health issues, including brain disease and eventually death, if untreated. It also increases the chances of acquiring and transmitting HIV.
According to Col. Amy Costello, chief of preventive medicine at the Air Force Medical Support Agency, STIs are easily transmitted.
“Chlamydia and gonorrhea are quite common; they can be transmitted vaginally, anally, or through oral-sexual contact,” she said in a Wednesday press release. “Pretty much any time you have mucous membrane contact with an infected person, you have a chance of getting it.”
Other Defense Department officials also expressed concern over the rise in STIs among servicemembers and the effect that it might have on military readiness.
“STIs place a significant economic strain on the US and military health care systems,” Maj. Dianne Frankel, an Air Force physician, said in the press release. Healthcare costs for STIs in the Navy alone in 2012 cost $5.4 million.
“From a military standpoint, STIs can have a significant impact on individual readiness, which in turn impacts unit readiness, which then leads to a decrease in force health protection,” Frankel added, also noting that STIs are likely on the rise due to high-risk behaviors among service members, such as having sex without a condom or having more than one sexual partner.
According to a 2015 Department of Defense Health-Related Behaviors Survey, one-fifth of those surveyed said they had more than one sexual partner in the last year, while one-third reported having had unprotected sex with a new partner. These statistics represent a fourfold increase since the previous survey in 2011, Frankel noted in the press release.
The rise in STIs may also be due to an increase in the use of dating apps, which “promote random, anonymous encounters, and when infections result, that anonymity can make partners difficult to track down,” the press release states. Other high-risk behaviors include having sex under the influence of drugs or alcohol, which can contribute to “greater sexual risk-taking” and “lower inhibitions.”
Studies have also shown that there is a high rate of alcohol use in the military, which is linked to less condom use and riskier sexual behavior. In addition, in a 2013 review of studies on STIs in the military, researchers at Brown University’s Women and Infants Hospital found out that servicewomen felt they would be perceived as sexually promiscuous if they insisted on condom use during a sexual encounter.