First Woman, Fourth Person Overall Cured of HIV Using Gene Therapy
00:40 GMT 16.02.2022 (Updated: 01:07 GMT 16.02.2022)
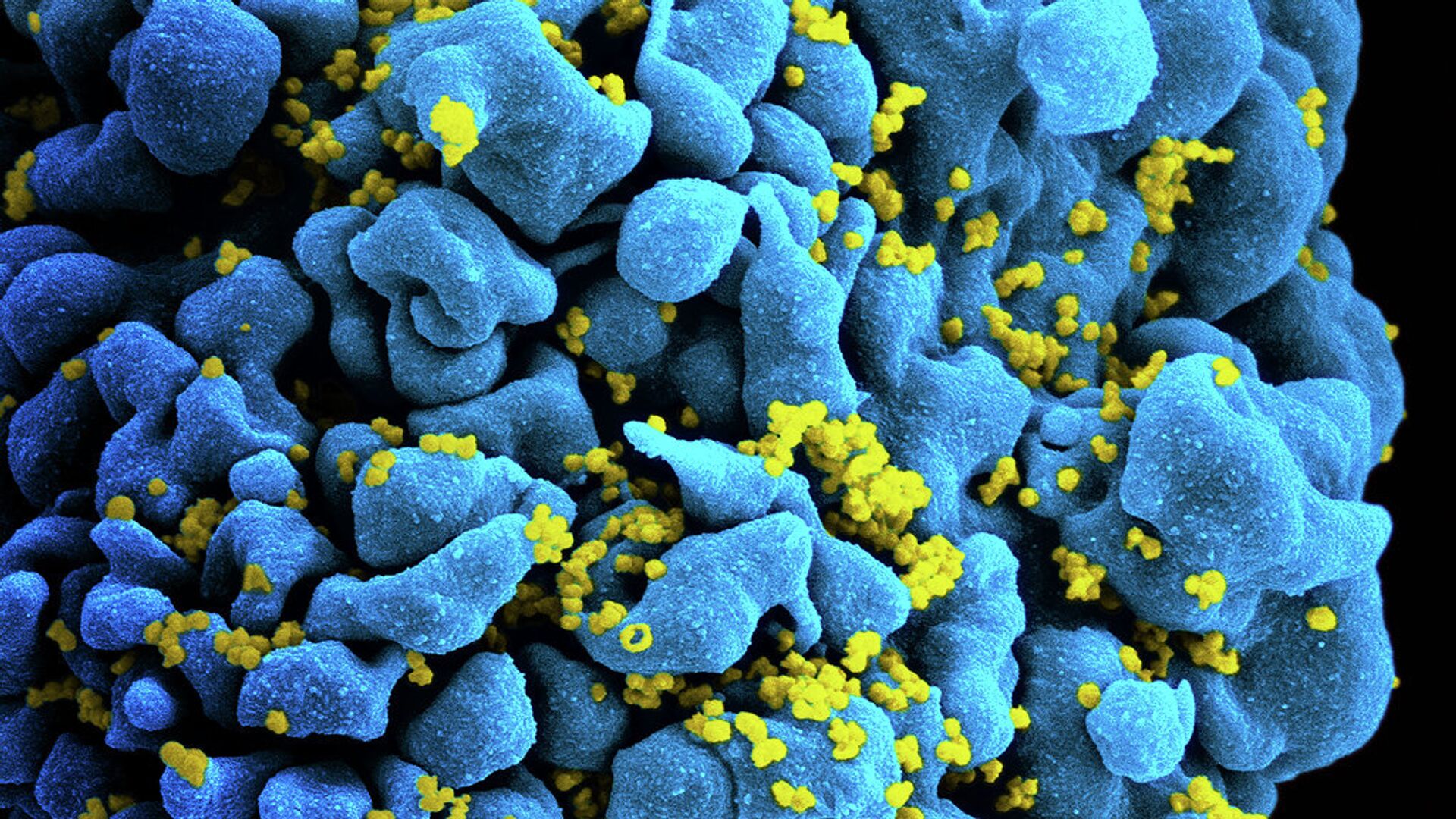
© Flickr / NIAID
Subscribe
A fourth person has achieved remission of Human Immunodeficiency Virus (HIV) infection following gene therapy and the ending of antiretroviral treatment. She is also the first woman to do so.
The woman, whose identity was not revealed by her doctors at New York-Presbyterian/Weill Cornell Medical Center in New York City, received stem-cell transplants from an adult relative and of umbilical cord blood from an unrelated newborn in order to treat acute myeloid leukemia, according to the Wall Street Journal (WSJ).
The sources weren’t random: the stem cells put into her body contained a genetic mutation that renders the CCR5 gene, a common entry point for HIV into the body’s immune system cells, impassable to the virus. If left untreated, a lengthy HIV infection can develop into Acquired Immunodeficiency Syndrome (AIDS) - a condition in which the virus has hamstrung the body’s immune system, meaning a typically minor infection can become life-threatening.
This patient is the first woman the procedure has ever worked in, but three other men have also achieved HIV remission following similar gene therapy treatments for blood cancers like leukemia. However, according to her doctors, the woman’s treatment process went considerably better than the men, who suffered major side effects; they credit her experience with the use of umbilical cord blood, the stem cells from which don’t have to be a perfect genetic match for the recipient.
However, she isn’t actually declared “cured” yet, as they need to wait and see if her infection returns. However, she stopped taking antiretroviral therapy, which HIV-positive people take in regular doses to keep their infections low, in October 2020. She received her transplant in August 2017
While the treatment is extremely specific and cannot be used to provide a general cure for the roughly 37.7 million people living with HIV, it could help scientists understand how to develop newer gene therapies that are “scalable” across larger populations and that use a patient’s own cells, which would be far safer, Steven Deeks of the University of California, San Francisco, told the WSJ.
HIV is known as one of the world’s most stubborn epidemic viruses, able to weather most treatments doctors have thrown at it. When it was identified in the early 1980s in the United States, it was found mostly among gay men and transgender women, the social stigmas of which led to years of indifference by medical professionals and national leaders, activists said at the time. Until an effective treatment was found in 1996, contracting HIV was seen by many as a death sentence.
Despite the drug’s discovery, HIV deaths did not peak until a decade later, as the treatment was extremely expensive in the First World and almost totally inaccessible in the Third, where the virus began to spread rapidly.
While many new drugs have been produced since then, which can block infection from occurring or suppress the virus to such low levels that patients are “functionally cured,” no true cure has ever been developed beyond the four gene therapy recipients.
According to the World Health Organization’s report on World AIDS Day on December 1, 2021, some 1.5 million people were newly infected with HIV in 2020 and 680,000 people died from HIV-related causes. Roughly 36.6 million have died from complications of AIDS since the epidemic began in 1981.
